98217 33877
info.secretarymus@gmail.com09 Jun 2018
Sonographic Diagnosis Of Occult Fractures

WHY NEGATIVE SKIAGRAM RESULTS
Inability to position the patient due to pain, bleeding, splints.
Young unco-operative patient /child
Special views not familiar, difficult to interpret
Severely osteoportic bones.
ROI inaccessible to the radiographic screens
Obese , physically challenged patient
Pregnant lady
Radiation risk
SONOGRAPHIC SIGNS OF OCCULT FRACTURES:
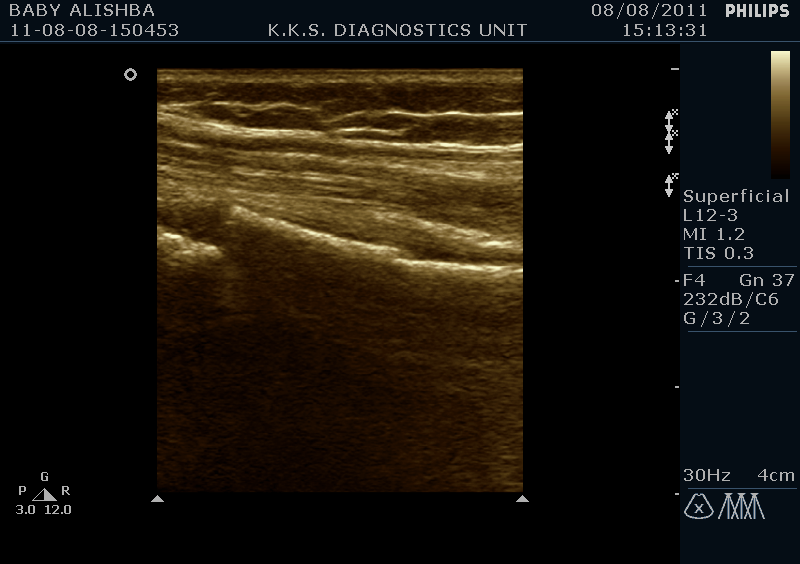
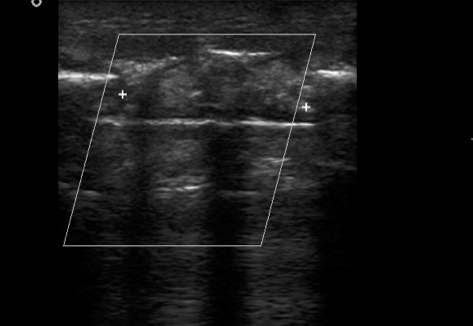
Step-off deformity.
Discontinuity of the cortical bone
Angulations of the bony contour
Sub-periosteal haematoma/ fluid
Callus formation.
Irregularity of the surface and contour of the bony prominences with h/o trauma.
Associated muscle hematoma.
Tenderness in the region of injury on sonographic palpation.
Impingement in the sub-acromial space due to fracture of greater tuberosity in occult fractures

How HFUS helps:
High frequency transducers.
USG is real time dynamic scanning with advantage of modifying the exam technique with tomographic images and contra-lateral comparison for normal.
Sonographic palpation is valuable in localizing the region of interest in long bones
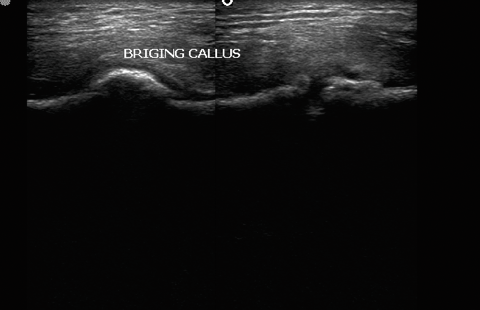
Callus formation helps to identify the region sometimes not seen on skiagrams
The most relevant features of MSK-US:
high patient’s acceptability (76%),
immediate diagnosis of joint and soft tissue disease (73%),
assessment of associated synovitis and tendons/tendon sheaths (73% and 70%),
Supports imaging guided joint injections/ aspirations and biopsies (67%).
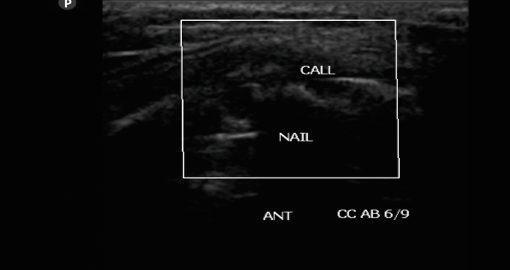
SONOGRAPHIC EVALUATION OF CALLUS
Cortical breach with intervening gap fills up with hypoechoic granulation tissue, evolving into bony matrix. This process is sonographically accessible to evaluation with greater accuracy and sensitivity in predicting optimal vs sub-optimal healing . Early intervention at 4-6 weeks post fracture can help reduce morbidity dramatically
Need for routine sonographic evaluation of fractures
Fractures notorious for non-union
For regions with Increased susceptibility to infection
Clinical suspicion of delayed union
Skiagram results sub-optimal
In Pediatric age group-ALARA
Post grafting /inadequate immobilization
Systemic causes of delayed or non-union
PEARLS:
EARLIEST PREDICTION OF DELAYED /NON-UNION AT 3-4 WEEKS
Correlative USG and patho-physiologic findings.
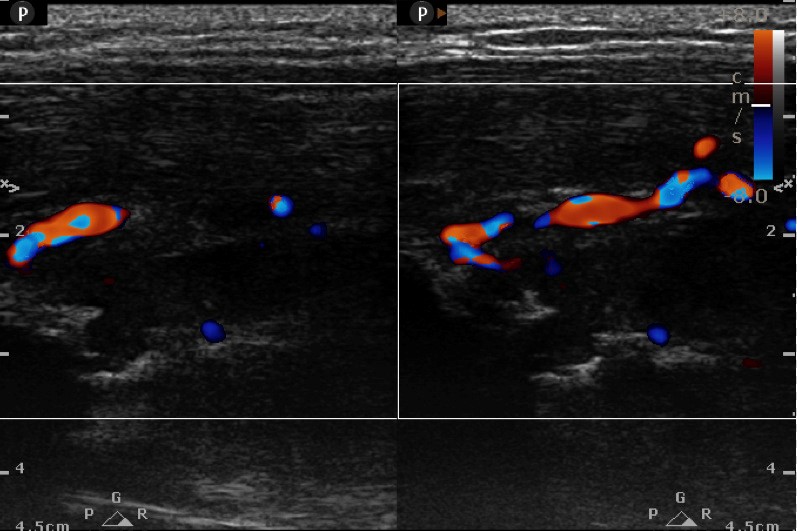
GRANULATION STAGE: soft hypoechoic callus + >5 vs + R.I. 0.50-0.70---2 wk
FIBROUS STAGE: Organized callus echo T.A.Ms. + vs ….3 wks
First screen USG at 4 weeks
CARTILAGENOUS STAGE: Long. oriented parallel to the fracture ends with speckled dots of mineralization+ vascularity…4 wk
OSSEOUS STAGE : Echogenic callus with acoustic shadowing and obscured medullary cavity / IM nail …5-6 wks
MSK USG has arrived but the world is yet to be taken by storm. It still remains an under-utilized modality because of MRI’s and hence the mind-set. Despite a myriad of advantages of ultrasound quoted, it probably lacks a uniformity because it is a highly observer dependent modality. But in competent hands it perhaps can give better and quicker results thereby improving patient care and a reduction in morbidity . Musculoskeletal system has long been equated with bones only and hence falsely understood as remaining elusive to ultrasound. High end ultrasound units and better understanding of the pathologies of MSK system have today made ultrasound as one of the very flexible and a useful modality since now it is understood that a bony pathology leads to cortical breach which creates an adequate window for assessing the pathological pattern without having to rush to MRI every time for an answer.
Fracture of long bones and in particular of tibia has remained a bane for most of the orthopedicians since they land up with frequent delayed and non-unions. Till date there is no modality except a skiagram which can predict union but not before 12 weeks... High frequency ultrasound has come to establish itself as the modality which can predict delayed union as early as 4 weeks and non-union at 7-8 weeks. Interlocking which is the mainstay of management for fracture shaft tibia today can be effectively managed early by dynamizing at 4weeks in case of delayed union , or in case of infections reaming with exchange nail at 6 weeks to save the patient the catastrophe of a non-union or osteomyelitis. Both grey scale imaging and colour doppler imaging act in a symbiotic manner to give a high predictability rate for union/ nonunion or delayed union in cases of fracture healing.